TRABAJOS ORIGINALES
Risk factors associated with infection in tibial open
fractures.
Marcos Almeida Matos1, Rômulo Neves Catro-Filho2, Bruno
Vieira Pinto da Silva2
Revista Facultad de Ciencias
Medicas 2013; 70(1):14-18
1. Bahian School of Medicine and
Public Health, Salvador-Bahia, Brazil;
2. Roberto Santos General Hospital, Salvador-Bahia, Brazil.
Conflict of interest:
None.
Corresponding Author:
Prof. Marcos Almeida Matos
Rua da Ilha, 378, Itapuã, Salvador-Bahia, Brazil, 41620-620
e-mail: malmeidamatos@ig.com.br
Tel(fax) 55-71-33588886
Introduction
The objective of the treatment of open fracture is to
prevent infection, stabilize the bones, and restore function.
However, preventing infection is the most important step in
achieving the latter aims.1-3
In the case of tibial open fractures, infection should be
prevented by prompt debridement within the first six hours (the
so-called “six-hour rule”) and early stabilization, if
possible1-3. Whether or not correct procedures are
followed, several clinical features can contribute to
infection and poor prognosis, including time delay for
debridement, severity of both lesions to bone and soft
tissues, other health conditions affecting the patients,
energy involved in the trauma and so on.1, 2, 4
The “six-hour rule” is based on experimental data5 and there
is no consensus among clinical studies that this rule
effectively diminishes the infection rate1,2,5,6,7,8,9,10.
Another problem is the large variety of methods used for
early stabilization in order to minimize the risk of
infection as well as to provide optimal recovery of
functioning4,7,9. Open fractures classifications such as the
Gustillo scheme11,13also try to improve the understanding
of how a fracture’s severity can lead to poor prognosis or
infection, but their ability to predict prognosis remains
uncertain.
For a surgeon and his patients, it is extremely important to
find out factors or clinical features that are able to
successfully predict an outcome. The control of those risk
factors, whenever possible, can lead to improvement of the
initial treatment in order to obtain the best
results1,2,11,12,13. The objective of this work is to find
risk factors associated with infection in a sample of tibial
open fractures.
Patients and Methods
A retrospective clinical analysis of patients who
underwent to tibial open fracture treatment in the Hospital
Geral Roberto Santos-HGRS, Salvador, Bahia, Brasil was
carried out. The study was conducted from March to October,
2009, and data was extracted from patient’s medical records.
All patients with an open tibial fracture were included.
Patients under the age of eight or having incomplete
information registered on their charts were excluded as well
as those suffering from systemic disease, metabolic bone
disease, or multiple fratures. Sample size was estimated to
be 48 patients based on an infection prevalence of 15%,
adopting a difference of 0.1 and an alpha error of 0.05.
In all cases, the initial treatment included careful
debridement using at least 10 liters of saline solution as
soon as possible, followed by antibiotic treatment for a
minimum of eight days. This is in accordance to the standard
Institutional protocol.
Clinical and demographic data were collected such as height,
weight, gender, age, marital status, origin, type and
characteristics of the trauma, time from trauma to
debridement (“time delay”), and type of stabilization.
Fracture type was assessed by AO classification11, and both
Gustillo grading system11 for open fractures and a modified
Tscherne grading system14 for soft tissue trauma were used
to evaluate the severity of the lesions.
Patient outcomes were divided into two groups: Group 1
comprises those without infection whereas group 2 comprises
those with lesions which became infected, both evaluated in
a period of one week after the trauma. Infection was
identified based on clinical and laboratory findings,
according to the criteria of early acute infection within a
period of two week proposed by Wielleneger15. That means we
count as infection any aspect of superficial or deep
infection associated or not with fever, high white blood
cell count or ESR6,15. The two groups were compared in
search for factors that could be associated with infection.
Statistical analysis
The data were described in percentages with CI95% for
nominal data, and in means ± sd for continuous data. The
association between group 1 and 2 were made by bivariate
risk analysis with OR and CI95% calculations, and tested by
chi-square test with Fischer and Yates correction. The value
<0.05 was adopted as the level of significance.
The study was approved by the Ethic Committee of the Bahian
School of Medicine and Public Health and also was approved
by the Institution, HGRS. The study was funded by the
involved Institutions.
Results
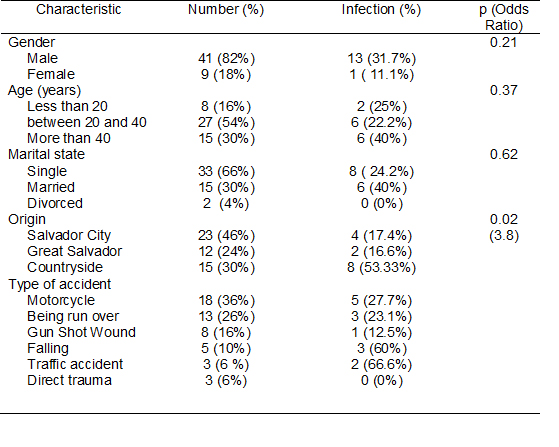
We studied 50 patients, divided into 41(82%;
CI95%=71.4-92.6) male and 9(18%; CI95%=7.4-28.6) female,
with an mean age of 32,9(±12,5) year old. Our overall
infection rate was 14 (28%; CI95%=15.5-40.5). The
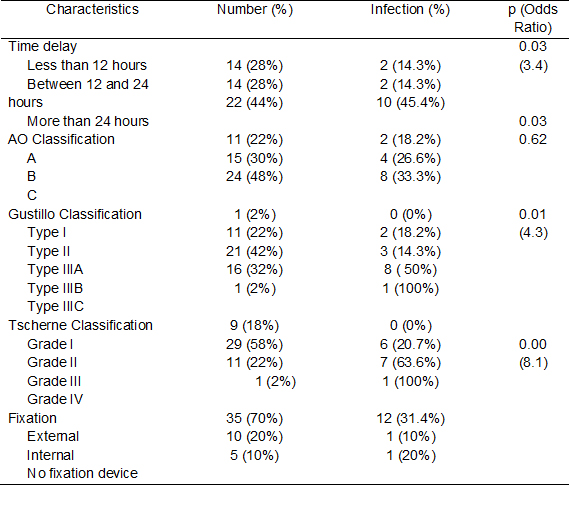
development of infection was significantly associated with
place of trauma (OR 3.78; CI95%=1.4-5.5; p=0.02), and a time
delay superior to 24 hours (OR 3.4; CI95%=1.4-20.8; p=0.03)
Infection was also related to the degree of soft tissue
damage and to bone fragmentation. Fractures graded as
Gustilo I, II and IIIA had a lower chance for infection
compared to Gustilo IIIB and IIIC (OR 4.32; CI95%=1.3-19.1;
p=0.01). Fractures graded Tscherne III and IV had a higher
chance for infection, and it was the most significant
isolated factor (OR 8.07; CI95%=2.4-47.1; p<0.00). We did
not find any association between infection and age, gender,
smoking, drinking, marital status or choice of stabilization
device. Data are shown in tables 1 and 2.
Discussion
Our overall infection rate was
14 (28% all percents should be have CI95%). Infection was
significantly associated with several characteristics of the
lesions such as place of trauma and Gustilo classification
system. We also presented a new relationship between soft
tissue and infection, and another relating time delay of
more than 12 hours with infection. Based on these findings a
time delay superior to 24 hours increases 3.4 times the
chance for infection, while fractures graded Tscherne III
and IV had also a chance 8.07 times higher for infection.
The infection rate in the present study was higher than most
previous studies. Harley et al (2002)2 presented an overall
infection rate of 9.3% and Spencer et al (2004)9 showed an
infection rate of 10.4%. We believe that this disagreement
was due to the clinical features of our sample. We had a
higher prevalence (76%) of grade III fractures, while these
authors had 30.2%2 and 49.5%9, respectively. With reference
to the prevalence of tibial fractures, Spencer et al (2004)9
had 35% and Harley et al (2002)2 had only 15%. Tibial
fractures have also higher infection rates due to the lack
of soft tissue coverage and to their poor vascularization7.
Therefore, the severity of the trauma associated with the
fact that our sample is comprised exclusively of tibial
fractures may have contributed to explain our infection rate.
Muller et al (2003)3 studied a sample comprised of 36%
tibial fractures and 54.6% Gustilo grade III fractures. That
study is more similar to ours and their results showed an
infection rate of 20.5%. On the other hand, Gustilo et al
(1984)16 and Muller et al (2003)3 showed infection rates of
63.1% and 48,8%, respectively, among grade III fractures.
Andrew et al (2010)10 have also shown an overall infection
rate of 27% while studying a sample of high-energy
fractures, including only those classified as grade III. All
those findings are in accordance with our results and
partially explain our higher infection rate.
The time between trauma and debridement in our series showed
a severe delay in the initial treatment (44% of our patients
were treated after 24 hours). The reasons for the prolonged
treatment times included late presentation, lack of hospital
beds, extended transportation time, patient instability
requiring neurosurgical or general surgical intervention,
and operating theater unavailability. Those problems are
relatively common taking into account that the Roberto
Santos General Hospital is a trauma referral center for a
vast geographic area and for a population close to 15
million people.
In the study performed by Spencer et al (2004)9, they found
that 60% of the patients were treated within 6 hours and
Harley et al (2002)2 found that only 47% of their patients
were treated within 8 hours. Both authors stated that time
delay in the treatment of open fractures is a common problem
in many general and referral hospitals2,9. Besides, most of
our patients came from the countryside, which means rural
trauma that occurs in areas far from cities, and it could
help to explain both the extensive delay in the treatment
and the higher infection rate.
The six-hour rule to debridement was based on historical and
laboratory data5. Only few recent clinical studies showed a
statistically significant association between infection and
time to debridement above 6 hours7,17. However, the study
performed by Kindsfater and Jonassen17 had an important
limitation taking into account that 17 (77%) of their grade
III fractures were in the delayed group (over 6 hours). On
the other hand, a large recent review of the orthopedic
literature wasn’t able to support the six-hour rule
theory1,2,4,9,18.
Based on the study conducted by Patzakis e Wilkins4 we
divided the patients into three groups: patients treated in
less than 12 hours, between 12 and 24 hours and after 24
hours from trauma time. Our results showed that up to a time
delay of 24 hours the infection rate is not significantly
increased. However, we find a 3.4 times higher chance for
infection in the group treated after 24 hours (45.4%). The
severity of the trauma in our sample associated with the
delay to treatment could have influenced our results. We
know that time was not an independent predictor of the risk
of infection10,18 alone. However, Andrew et al (2010)10
found that their patients treated within three hours had an
infection rate of 17% and those treated after eleven hours
had a significant higher rate of 36.1%; their samples was
made up exclusively of severe cases (grade III). Our
findings support Andrew´s study as well as the idea that
time may be an important predictor of infection in severe
fractures (grade III).
We advocate for debridement as early as possible as the best
choice in treating open fracture and we do not believe that
our findings can justify any delay. Moreover, debridement
gives the surgeon an idea of how important the factor time
is when planning the procedure. Spencer et al9 stated that
emergency surgeries based exclusively on the “six-hour” rule
can lead to procedures done in the worst-case scenario with
regard to the orthopedic team, adequate synthesis material
and a patient’s health conditions. Our findings also
indicate that when the six-hour rule is not the most
important point to consider, in some complex cases better
results could be achieved if the surgery can be planned more
adequately and carefully within 24 hours.
In the present study, Gustillo’s classification11 was able
to predict infection (OR 4.33) and the same relationship was
not obtained with respect to AO classification12. The
association between Gustilo’s classification and infection
has been emphasized by several authors. In the study
performed by Kathod et al7, for instance, they found
infection rates as follows: 8.7% (in type I), 10.9% (in type
II), 23.5% (in type IIIA), 67.7% (in type IIIB), and 62.5%
(in type IIIC). These findings are very similar to ours (Table
2), despite the fact that our sample was comprised by more
severe cases and a more prolonged time delay.
The use of Gustilo’s classification system is widespread and
well-accepted. However, its agreement rate is significantly
low (60%)19 and the system may not show the real extent of
soft tissue involvement11,17,19. The Tscherne system12, on
the other hand, is solely based on soft tissue lesion and
represents a new approach to open fractures. In our study,
Tscherne’s classification showed a better relation to
infection than any other risk factor alone (OR 8.07). It
suggests that damage to soft tissue alone could be the most
important risk factor for a poor prognosis, but we did not
find similar papers so that we could discuss this issue in
depth. Further studies would be necessary to confirm or not
these findings.
The present study has some strong points that made our
results more significant. Our data represents a homogeneous
sample comprised exclusively by tibial open fractures and
focuses on what happens in more severe cases, most of which
were treated after a six-hour period. The weak point is that
we did not study infection in the long run, after hospital
discharge. Eventually, the findings of our study could have
been influenced by small sample size, and information bias
because it was based on retrospective design (medical
records). Therefore, our results must be confirmed by other
similar studies.
The study contributes significantly to the current
literature about risk factors for infection in tibial open
fractures. We confirmed the relationships between infection
with Gustilo classification and trauma from the countryside.
We also presented new relationships between soft tissue
damage and infection, and another relating time delay of
more than 12 hours with infection.
Tablas
|
 |
 |
|
|
Table 1- Social, demographic and
characteristics of the
trauma in the whole group.
|
Table 2 – Characteristics of the
injury and Treatment |
|
References
1.
Ashford RU, Mehta JA, Cripps R: Delayed presentation is no
barrier to satisfactory outcome in the management of open
tibial fractures. Injury; 2004,35:411-6.
2. Harley BJ, Beaupre LA, Jones CA, Dulai SK, Weber DW: The
effect of time to definitive treatment on the rate of
nonunion and infection in open fractures. J Orthop Traum;
2002,16:484-90.
PubMed
3. Muller SS, Sardenberg T, Pereira GJC, Sadatsune T, Kimura
EE, Novelli-Filho JLVB: Epidemiological, clinical and
micorbiological prospective study of patients with open
fractures assisted at a university hospital. Acta Ortop Bras;
2003,11:158-169.
Scielo
4. Patzakis MJ, Wilkins J: Factors influencing infection
rate in open fracture wounds. Clin Orthop Relat Res;
1989,243:36-40.
PubMed
5. Friedrich PL: Die aseptische Versorgung frischer Wundern.
Arch Klin Chir; 1989,57:288-310.
6. Garner JS: CDC guideline for prevention of surgical wound
infection. Infect Control; 1985,7:190-200.
7. Khatod M, Botte MJ, Hoyt DB, Meyer RS, Smith JM, Akeson
WH: Outcomes in open tibia fractures: relationship between
delay in treatment and infection. J Trauma; 2003,55:949-54.
PubMed
8. Skaggs DL, Friend L, Alman B, Chambers HG, Schmitz M,
Leake B, Kay RM, Flynn JM: The effect of surgical delay on
acute infection following 554 open fractures in children. J
Bone Joint Surg Am; 2005,87:8-12.
PubMed
9. Spencer J, Smith A, Woods D: The effect of time delay on
infection in open long-bone fractures: a 5-year prospective
audit from a district general hospital. Ann R Coll Surg Eng;
2004,86:108-12.
Full. Text
10. Pollak AN, Jones AL, Castillo RC, Bosse MJ, MacKenzie EJ:
The Relationship Between Time to Surgical Debridement and
Incidence of Infection After Open High-Energy Lower
Extremity Trauma. J Bone Joint Surg AM; 2012.92:7-15.
Full Text
11. Gustilo RB, Anderson JT: Prevention of infection in the
treatment of one thousand and twenty-five open fractures of
long bones: retrospective and prospective analyses. J Bone
Joint Surg Am; 1976,58:453-8.
PubMed
12. Müller ME: The comprehensive classification of fractures
of long bones. In: Müller ME, Allgöwer M, Schneider R,
Willeneger H. Manual of internal fixation. 3th ed. Springer-Verlag,
Berlin. 1992;p.118-50.
13. Papakostidis C, Kanakaris NK, Pretel J, Faour O, Morell
DJ, Giannoudis PV: Prevalence of complications of open
tibial shaft fractures stratified as per the Gustilo-Anderson
classification. Injury; 2011,42:1408-15.
PubMed
14. Oestern H-J, Tscherne H:Pathophysiology and
classification of soft tissue injuries associated with
fractures. In: Tscherne H. Gotzen L, Eds. Fractures with
soft tissue i njuries. Springer-Verlag, Berlin. 1984;p.1-8.
15. Willenegger H, Roth B: Treatment tactis and late results
in early infection following osteosynthesis.
Unfallchirurgier; 1986,12:241-6.
16. Gustilo RB, Mendoza RM, Williams DN: Problems in the
management of type III (severe) open fractures: a new
classification of type III open fractures. J Trauma;
1984,24:742-6.
PubMed
17. Kindsfater K, Jonassen EA: Osteomyelitis in grade II and
III open tibia fractures with late debridement. J Orthop
Traum; 1995,9:121-7.
PubMed
18. Schlitzkus LL, Goettler CE, Waibel BH, Sagraves SG,
Hasty CC, Edwards M, Rotondo MF: Open fractures: it doesn't
come out in the wash. Surg Infect; 2011,12:359-63.
PubMed
19. Brumback RJ, Jones AL: Interobserver agreement in the
classification of open fractures of the tibia. The results
of a survey of two hundred and forty-five orthopaedic
surgeons. J Bone Joint Surg Am; 1984,76:1162-6.
PubMed
|